Despite Having Heart Attack, Many Smoke, Are Obese
STORY HIGHLIGHTS
- Those who have had a heart attack less likely to exercise than those who haven’t
- Those who have survived a heart attack more likely to experience stress
- Eating habits similar among those who have and haven’t had a heart attack
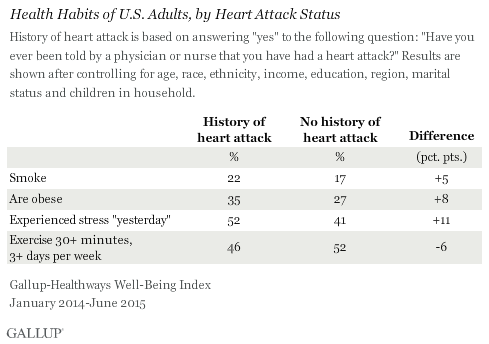
WASHINGTON, D.C. — Americans who have had a heart attack may not be making the necessary lifestyle changes to reduce their risk of having another one. Those who have had a heart attack are significantly more likely than those who have never have had a heart attack to smoke, be obese and experience stress. And those who have survived a heart attack are much less likely to exercise regularly.
Medical research shows that patients who have had a heart attack are at higher risk for having another one. While individuals cannot change some risk factors for having a heart attack — increasing age, being male, hereditary factors and having a family history of heart disease — they can make lifestyle changes that may reduce their risk for, or even reverse, cardiac disease. These changes include eating a heart-healthy diet; engaging in regular, moderate physical activity; quitting smoking; maintaining a healthy weight; and minimizing stress.
These findings, collected as part of the Gallup-Sharecare Well-Being Index from January 2014 through June 2015, do not follow the same people over time and cannot speak to whether those who have had a heart attack are practicing healthier behaviors than they were before they had a heart attack. It is possible that, as a group, those who have had a heart attack at some point in their lifetime have healthier habits now than they did before they had a heart attack. But these findings do show that, overall, Americans who have survived a heart attack are still less likely to practice key healthy behaviors than those who have not had a heart attack.
Even after controlling for key demographic differences between those who have had a heart attack and those who haven’t — such as age, race or ethnicity, gender and income — these differences hold.

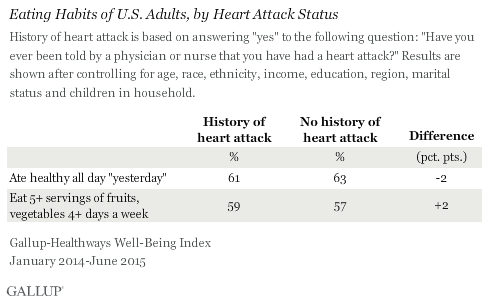
Self-Reported Eating Habits Similar for Both Groups
While those who have had a heart attack fall short on a number of important healthy behaviors, their self-reported eating habits are similar to those of Americans who have not had a heart attack. Both groups are about as likely to say they practiced healthy eating all day “yesterday” and to say they eat the recommended number of servings of fruits and vegetables each week.
Still, about two in five people who have had a heart attack say they did not practice healthy eating the day before being interviewed and that they do not consume the recommended amount of fruits and vegetables.
On a positive note, nine in 10 people who have had a heart attack say they have a personal doctor, higher than the 83% found among those who have not had a heart attack. This is an encouraging sign that those who have had a heart attack may have a physician regularly monitoring their cardiac health and helping them manage their risk for another heart attack.
Implications
The percentage of U.S. adults who report having had a heart attack has declined over the seven years Gallup and Sharecare have measured it, from 4.5% in 2008 to 3.9% in 2014. While the overall drop in this figure is positive news, many people who have had a heart attack may not be making the lifestyle changes that could prevent or reverse cardiac disease, given their higher smoking and obesity rates, higher stress levels and poorer exercise habits compared with those who have never had a heart attack. Not making these lifestyle changes could lead to higher healthcare costs and utilization, putting a financial strain on the economy, healthcare systems and families.
The percentage who report having had a heart attack varies widely by state — from a low of 2.4% in Utah to a high of 7.7% in West Virginia. Hospitals, employers and insurance companies, especially those in states with high percentages of residents who report that they have had a heart attack, can provide heart attack survivors and those at risk with the ongoing education, resources and support they need to help them make positive changes. And given that nine in 10 Americans who have experienced a heart attack report having a personal doctor, physicians are uniquely positioned to reinforce the lifestyle changes patients should make to prevent another heart attack.
“Heart disease is preventable and usually even reversible for most people by making comprehensive lifestyle changes — eat well, stress less, move more, love more,” said Dr. Dean Ornish, president of the Preventive Medicine Research Institute. “A new paradigm of healthcare — lifestyle medicine — empowers people to address and transform these underlying causes of heart disease.”
Family and friends also can play an important role in encouraging those who have had a heart attack to improve their health habits. Previous Gallup and Sharecare research shows that having a heart attack doubles the odds of being diagnosed with depression. People who have had a heart attack often need social support to manage the numerous lifestyle changes they need to make and to cope with the depression and stress that can accompany such a major health event.
Ultimately, though, it is up to those who have had a heart attack to commit to lifestyle changes that could prevent further heart disease — not just immediately after a heart attack, but for the rest of their lives.
Read more about heart attack rates by state.
SURVEY METHODS
Results are based on telephone interviews conducted Jan. 2, 2014-June 30, 2015, as part of the Gallup-Sharecare Well-Being Index survey, with a random sample of 265,369 adults, aged 18 and older, living in all 50 U.S. states and the District of Columbia. For results based on the total sample of national adults, the margin of sampling error is ±0.24 percentage points at the 95% confidence level. For results based on the total sample of people who have had a heart attack, the margin of sampling error is ±1.08 percentage points at the 95% confidence level. All reported margins of sampling error include computed design effects for weighting.
Each sample of national adults includes a minimum quota of 50% cellphone respondents and 50% landline respondents, with additional minimum quotas by time zone within region. Landline and cellular telephone numbers are selected using random-digit-dial methods.
Learn more about how the Gallup-Sharecare Well-Being Index works.