U.S. Obesity Rate Inches Up to 27.7% in 2014
Reposted with permission from Gallup
STORY HIGHLIGHTS
- Obesity rate up from 27.1% in 2013 and 25.5% in 2008
- Obesity rate increased most among Americans aged 65+ since 2008
- Americans who are obese have lower well-being
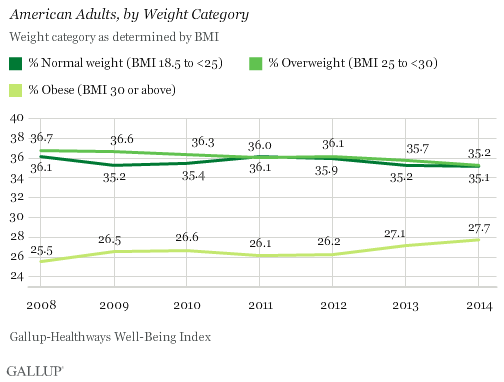
WASHINGTON, D.C. — The percentage of U.S. adults who are obese continued to trend upward in 2014, reaching 27.7%. This is up more than two percentage points since 2008 and is the highest obesity rate Gallup and Sharecare have measured in seven years of tracking it. More Americans who were previously overweight have now moved into the obese category, while the percentage who are at normal weight has remained stable since 2013.
The percentage of Americans who are underweight has remained steady at 2.0%.
These results are based on more than 167,000 interviews conducted in 2014 as part of the Gallup-Sharecare Well-Being Index. Unlike government estimates of obesity, the Gallup-Sharecare Well-Being Index uses respondents’ self-reported height and weight to calculate body mass index (BMI). The Centers for Disease Control and Prevention and government estimates of obesity are slightly different, as they are calculated using clinical measurements of height and weight as part of the National Health and Nutrition Examination Survey (NHANES). The latest NHANES results from 2011-2012 reported a 34.9% obesity rate for adults aged 20 or older, not significantly different from data collected since 2003. Another self-reported government survey, the Behavioral Risk Factor Surveillance System, says the obesity rate for U.S. adults aged 18 and older was 29.4% in 2013.
Individual BMI scores of 30 or above are classified as “obese,” 25 to 29.9 are “overweight,” 18.5 to 24.9 are “normal weight” and 18.4 or less are “underweight.” While the Gallup-Sharecare data show that just more than 35% of Americans have been classified as “normal weight” from 2008 to 2014, the obesity rate has risen each year except 2011, with at least a quarter of adults having BMIs categorized as obese.
More Americans Now Classified as Morbidly Obese
The World Health Organization further classifies BMI scores of 30.0 or higher into three classes of obesity:
- Obese class I = 30.0 to 34.99
- Obese class II = 35.0 to 39.99
- Obese class III = 40.0 or higher
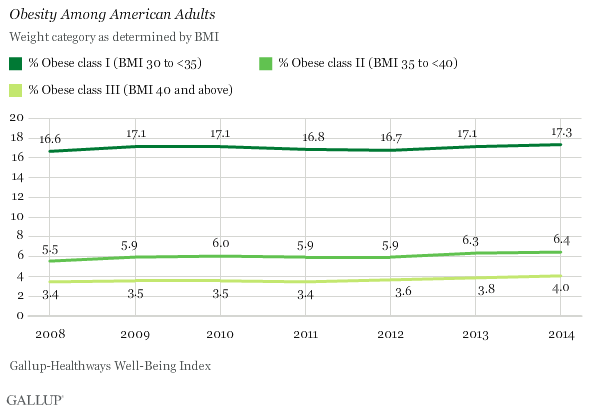
Those with BMIs of 40.0 or higher — obese class III — are often considered “morbidly obese.” According to Americans’ self-reports of height and weight, the 4.0% who are classified as morbidly obese in 2014 is the highest Gallup and Sharecare have measured in seven years of tracking.
The percentage of Americans in obese class I and obese class II have also increased slightly since 2008. The marginal increases across all three obesity classes have potentially negative consequences as healthcare costs related to obesity continue to rise.
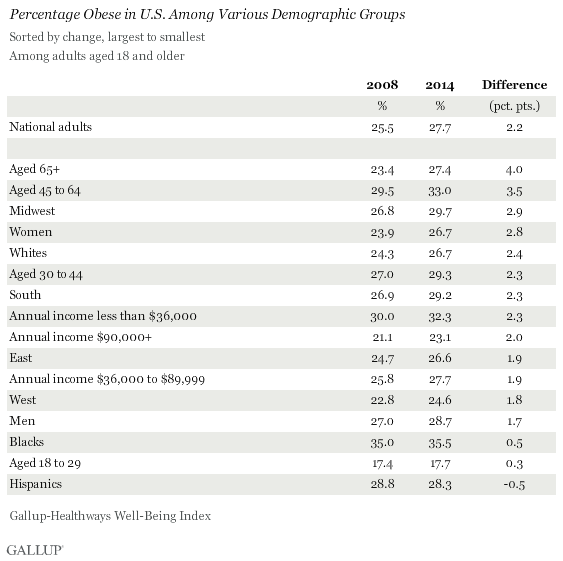
Obesity Rises Most Sharply Among Seniors Since 2008
Obesity rates have increased at least marginally in 2014 compared with 2008 across nearly all major U.S. demographic groups. Since 2008, Americans aged 65 and older have seen the sharpest uptick in obesity, a four-percentage-point increase to 27.4%. This is followed by increases among 45- to 64-year-olds (3.5 points), Americans living in the Midwest (2.9 points) and women (2.8 points). Obesity rates among Hispanics, blacks, and young adults aged 18 to 29 are similar to those found in 2008.
Although the obesity rate among blacks has not changed much since 2008, this group has the highest obesity rate of any major demographic group, at 35.5%. Obesity rates also exceed 30% among Americans aged 45 to 64 and those earning less than $36,000 per year. Young adults aged 18 to 29 are the least likely to be obese (17.7%), followed by those earning at least $90,000 per year (23.1%).
Excess Weight Linked to Lower Overall Well-Being
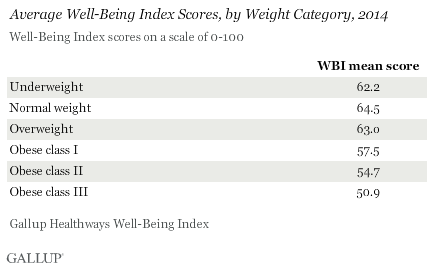
Americans of a normal weight have the highest average well-being (64.5), followed by those who are overweight but not obese (63.0). Underweight Americans (62.2) have lower well-being than those who are overweight. Americans who are obese have the lowest well-being across weight groups.
As Americans become more obese, their well-being declines significantly, as measured by Gallup-Sharecare Well-Being Index scores. Adults in obese class III, those considered morbidly obese, had the lowest average well-being of any weight group, at 50.9, in 2014. This compares with 54.7 for those in obese class II and 57.5 for those in obese class I.
The Gallup-Sharecare Well-Being Index measures the five essential elements of well-being: purpose, social, financial, community and physical. The Well-Being Index is calculated on a scale of 0 to 100.
Implications
While it is well-known that obesity is associated with physical health problems such as diabetes, high blood pressure and other chronic diseases, obesity is also linked to other elements of well-being. Gallup previously found that obese adults experience lower social well-being than their normal-weight or overweight counterparts. Furthermore, higher obesity rates are linked to lower incomesand long-term unemployment, suggesting a relationship exists between obesity and lower financial well-being.
While the relationship between well-being and obesity is reciprocal, previous Gallup research demonstrated that overall well-being influences future obesity outcomes more than obesity influences future well-being. Regardless of the direction of the relationship, this research suggests that helping Americans move from the obese to the overweight and normal weight categories would boost the overall U.S. economy. In addition to reducing healthcare costs, previous Gallup research shows that higher well-being predicts key business outcomes such as lower absenteeism and turnover, as well as fewer workplace safety incidents.
With the obesity rate increasing across nearly all demographic groups since 2008, it is imperative for employers, public health officials and individuals themselves to act to reverse the trend. However, given the link between lower well-being and obesity, these actions should focus on more than just diet and exercise.
“To date, most efforts to curb obesity focus on driving weight loss through diet and exercise, without addressing other aspects of well-being that may contribute to obesity,” said Janna Lacatell, Sharecare Lifestyle Solutions Director. “The rising obesity rate suggests these efforts have been largely ineffective. While access to evidence-based, proven weight loss programs emphasizing better nutrition and more physical activity is a critical component to reducing obesity, these interventions alone are not enough. To make a truly measurable impact on reducing obesity rates, interventions should also address other factors known to influence weight management, such as financial and social well-being.”
Addressing the underlying causes of obesity through a better understanding of all elements of well-being can help more Americans achieve a long-term healthier weight.