Depression Risk and Financial Health are Intrinsically Connected
Long before COVID-19 gripped the world, the cyclical link between depression risk and financial health was well-established: Poor financial health causes stress and anxiety that can worsen mental health; mental health problems in turn negatively affect physical well-being and productivity1, making it more difficult to manage and earn money.
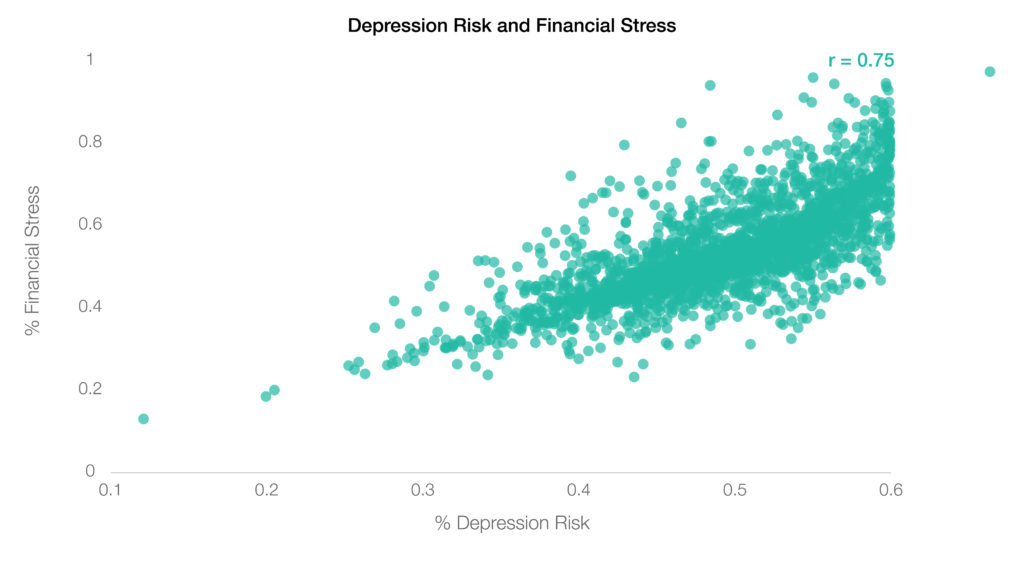
Communities with the greatest levels of financial stress in 2020 represented more than 1.5 times the depression risk measured in communities with the lowest levels of financial stress, according to the latest findings from Sharecare’s Community Well-Being Index. The Index found that more than three in five people screen positively for depression risk in communities with the greatest financial stress, compared to two in five in communities with the lowest levels of financial worry and insecurity.
Moreover, Index research established significant relationships between depression risk and financial stress at the county level (below), linking mental and financial health with geography. These findings underscore prior research that demonstrates the relationships between stable finances and enhanced mental resilience with greater access to resources and improved infrastructure.
Financial Well-Being Declines During the Pandemic.
Financial stress was not uncommon prior to the pandemic. Index results from 2018 showed that only four in 10 Americans agreed that they had been free from money worry in the last seven days, and fewer than two in 10 agreed that they were satisfied with their standard of living. These pre-pandemic findings suggest that a large percentage of the population had already been experiencing financial stressors and discomfort before the onset of COVID-19.
During the pandemic, these already-concerning levels of financial stress and worry increased, contributing to broad declines in financial well-being across the country. This heightened financial strain triggered concerns tied to downstream depression and overall health risk. This is particularly evident in communities with the lowest levels of resources, access, and economic stability.
Depression Risk Rises – Enhanced Risk for Underserved Communities.
Over the course of 2020 and into this year, multiple bodies of research have realized these concerns.
Boston University School of Public Health (BUSPH) research published in The Lancet Regional Health – Americas found that symptoms of depression increased from 27.8% in 2020 to 32.8% in 2021. The survey responses showed that depressive symptoms intensified over time and continue to remain high at the population level. Those who have lower household income and have experienced COVID-19 related stressors — including job loss, financial problems, difficulty paying rent, inability to get food due to shortages, and/or not being able to get supplies due to shortages — are among those most affected, according to lead author Catherine Ettman, a doctoral candidate at the Brown University School of Public Health and chief of staff and director of strategic initiatives in BUSPH’s Office of the Dean. “The sustained and increasing prevalence of elevated depressive symptoms suggests that the burden of the pandemic on mental health has been ongoing—and that it has been unequal,” says Ettman, noting that efforts moving forward should keep in mind low-income populations who have been disproportionately affected by the pandemic.
Building on BUSPH findings, Sharecare’s Community Well-Being Index assessed commonalities among areas with the highest and lowest risk for experiencing severe depression symptoms in 2020. In general, the Index revealed that areas with the lowest percentage of residents who reported severe depression risk had enhanced levels of social determinants of health. In particular, areas with the lowest levels of depression exhibited:
- 1.5x more MDs
- 1.6x fewer residents living in poverty
- 2.4x higher percentage of residents who take public transit to work
- 1.4x more residents with a college degree
- 1.7x lower percentage of households receiving the federal Supplemental Nutrition Assistance Program (SNAP)
Sharecare also evaluated the perennial relationship between financial stress, depression risk, and overall community well-being, noting that states with the greatest financial stress also exhibited the greatest levels of depression risk and some of the lowest overall community well-being.
“States like Mississippi, New Mexico, Louisiana, and Oklahoma exhibited both the highest financial stress and the greatest depression risk according to 2020 findings, coinciding with low rankings in measures of well-being, as well as low rankings in social determinants across economic security, food access, and housing and transportation,” says Michael Rickles, PhD, VP, Research for Sharecare’s Community Well-Being Index. “While these relationships are not new, we now know that declines in mental and financial health are hitting the geographies and subpopulations with the least access and infrastructure in place. It’s concerning enough for these issues to be pervasive in populations of privilege, so for underserved communities, this could certainly be the next major crisis we face.”
Turning Data into Action
With broad declines in financial and mental health, as well as enhanced risk for underserved populations and communities, it is critical that both individuals and organizations take action to mitigate risks stemming from both individual behaviors to the communities where they live, work, and play.
“Since we need money to survive in modern society, the thought of not having enough to buy food or pay rent can trigger stress and anxiety. In that moment, it really can feel like it’s ‘life or death’. And since bills are always due, the stress never really goes away. Over time, it can build into deep anxiety about your finances. By bringing in mindfulness practices, like curiosity and kindness, we can help alleviate some of that stress and anxiety.” says Jud Brewer, MD, PhD, an associate professor of Behavioral and Social Sciences at Brown University’s School of Public Health.
In addition, governments, healthcare providers, and organizations can help people attain financial and mental resilience by first understanding the incidence of depression and financial health risk among their populations. They should connect people with targeted health-promoting platforms, including care advocacy programs that guide individuals through everything from educational content to nearby healthy actions, healthcare resources and financial wellness programs.
Sharecare’s Index found that while nearly 50% of Americans exhibited severe depression symptoms in 2020, only 6% reported a clinical diagnosis for depression. Despite being one of the most treatable mental health conditions, with 80% to 90% of people with depression eventually responding well to treatment, clear gaps in care persist. Care advocacy solutions can both identify mental health risk and help individuals navigate their care options.
Organizations should also support underserved populations, including specific assessment health equity considerations and community-based initiatives that promote healthy behaviors and environments.
“Leaning in on mental and financial health and understanding how it connects to constituents’ everyday lives will be paramount in developing post-pandemic healthy workforces and communities,” says Rickles. “And while we recommend a multi-faceted approach to resilience at the individual and community level, including digital, high-touch, community, and in-home protocols, taking action can be as simple as connecting to local community-based organizations.”
Mental Health Resources
If you believe that you or someone you know is at risk for suicide, reach out for help. Anyone considering suicide can contact the Crisis Text Line by texting ‘HELLO’, ‘HOME’, START’ or ‘NAMI’ to 741741. They will be connected with a person who will listen to their concerns without judgement. They can also call the National Suicide Prevention Lifeline at 1-800-273-8255.
1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3062016/